Member ID

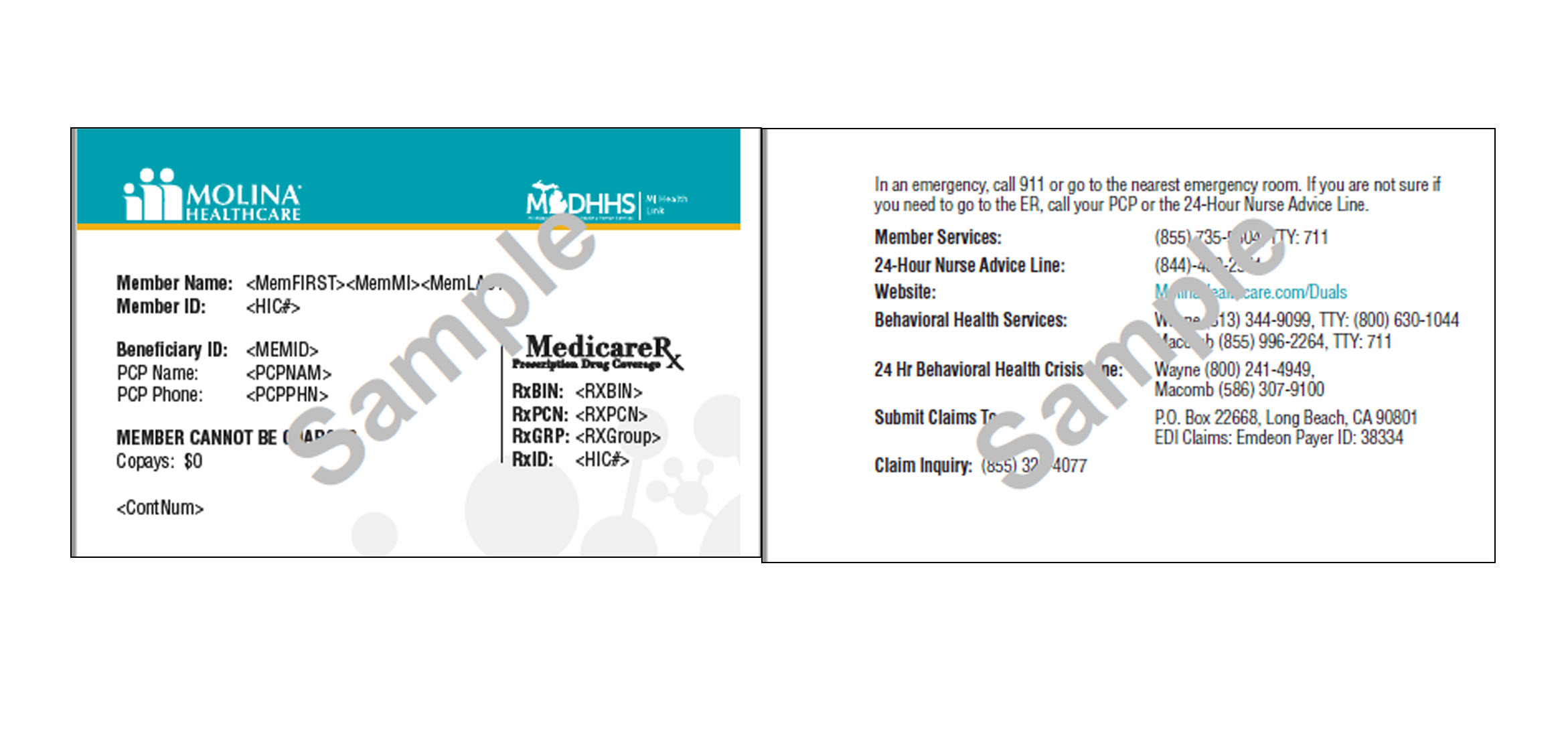
You will no longer need to carry both your Medicare ID card and your Medicaid information when getting medical services. Now all the information you need to show you qualify for benefits will be on just one card. Your Molina Dual Options MI Health Link ID card will also include important phone numbers and prescription information to help you get your medicine.
You should receive your Member Handbook and Molina Dual Options MI Health Link ID Card a week or two after your enrollment is effective.
As a member of Molina Dual Options, you must use your membership card when you get any services covered by this plan, and when you get medication at network pharmacies.
If your plan membership card is damaged, lost, stolen, or if you want more information, call Member Services. We will send you a new one. You can also request for a new card online at My Molina.